
Best Dermatology Clinic in Pune
The Department of DERMATOLOGY in Holistic Hospital is committed to providing specialized treatments and excellent comprehensive care for our patients. The Department of DERMATOLOGY is well equipped with State of the ART lab facilities and Experienced Clinical Team.
Dermatology is the branch of medicine that deals with skin, nails, hair and its diseases. It is a specialty with both medical and surgical aspects. A dermatologist treats ailments and some cosmetic problems of the skin, scalp, hair, and nails. A dermatologist can help in improving complete appearance of a person with a lot of confidence counselling. Here are few treatments provided in the department of dermatology at Eternis Clinic:
Treatment of Dermatology
What is Acne?
Acne is a chronic inflammatory disease of the sebaceous hair follicles often referred to as pimples or zits. This usually appears on the face, neck, back, chest, and shoulders. It can be a source of emotional distress, and severe cases can lead to permanent acne scars.
How does it form?
Each follicle contains a tiny hair and multiple sebaceous glands. Under normal circumstances, sebum, the oily substance made by the sebaceous glands, travels up the hair follicle and out to the skin`s surface. Acne is caused by an excessive amount of abnormal oil production, blockage of the openings to the oil producing glands (resulting in tiny blackheads) and also due to a bacterium, Propionibacterium acnes (P. acnes) which causes inflammation in the blocked glands.
Who gets Acne?
Anyone can have acne at any age, but teenagers are most prone because of the surging adolescent hormone levels. Under influence of these hormones oil glands produce excess oil.
What are the factors precipitating Acne?
- Hormonal changes during Pregnancy, stress and just before menses
- Oily Comedogenic Cosmetics or hair products
- Oral Medicines containing Steroids, testosterone, Estrogens
- Food – Whey proteins, Oily & Dairy food products
- Environmental Factors – Excess Sun exposure & sweating, high humidity
- Medical conditions like PCOS, SAHA syndrome, Hyperprolactinemia
How can it be treated?
Almost all cases of acne can be effectively treated. The goal of acne treatment is to heal existing lesions, stop new lesions from forming, and prevent acne scars. Treatment varies from topical medications alone to oral medicines along with Chemical peels and laser treatments. So treatment depends on the type of your skin and acne severity.
How long do I have to take treatment?
Unfortunately there is no fixed duration of treatment for acne. Once your acne is under control (which may take few months), a maintenance therapy is advised which aims at preventing new lesions. Stopping treatment on your own after initial response, may lead to recurrence of acne.
Skin care tips for Acne Prone Skin
- Keep your face clean off dirt and oil with mild cleanser
- Make sure not to touch and pick the pimples.
- Use clean towels while wiping your face (Not vigorously)
- Ensure that pillow you use has a clean cover that is washed at regular intervals
- Eat Fresh and healthy food. Avoid oily and junk Food. Limit dairy food intake (Including Chocolates)
- Stay away from direct sunlight as much possible. Cover yourself properly with non oily sunscreen and umbrellas when you go out
- Use Skin care products, Makeup and cosmetics labeled as “non-comedogenic” (means it does not promote acne)
- Always follow treatment protocols given by your dermatologist
What are Acne Scars and how do they occur?
Acne scars are depressions (pits) or elevations in the skin that are left behind once acne lesion is cleared. Inflammation at the site of acne causes damage to skin and surrounding structures. This leads to replacement of healthy collagen by unhealthy scar tissue forming either depressed (atrophic) or elevated (hypertrophic) scars.
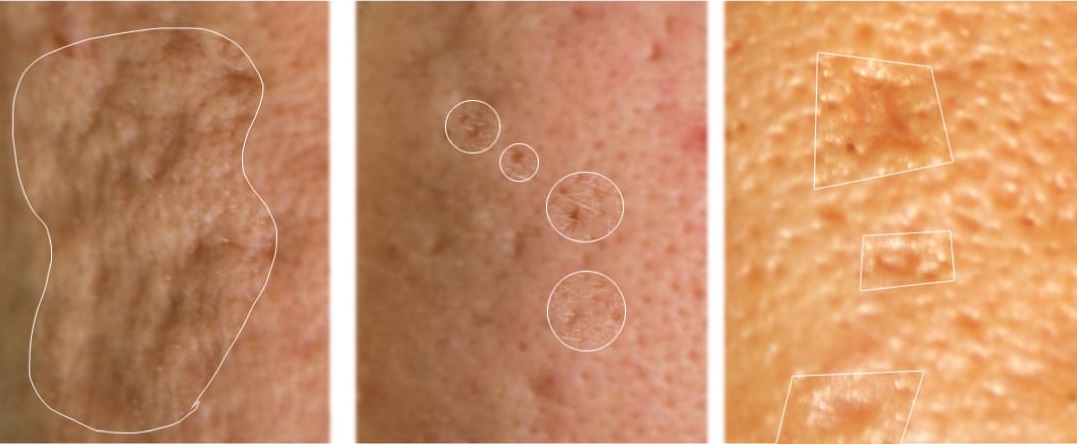
How do I get rid of acne scars?
Treatment of acne scars is challenging. It requires expertise on dermatologist’s side and patience on patient’s side. It is a multipronged individualized approach depending on type of scars, its duration, type of skin and skin colour. Consult your dermatologist to decide best management approach. Multiple procedures used to treat acne scars are
- Professional Peels
- Microdermabrasion
- Micro-needle therapy
- Platelet rich plasma (PRP)
- Lasers – Fractional Co2 laser
- Ablative Radiofrequency
- Scar surgeries like subcision, punch excision and suturing
Hypertrophic Acne Scars and Keloids
Sometimes acne lesions may heal abnormally to form elevated or hypertrophic scars. Keloids are hypertrophic scars which spread beyond their boundaries and are mostly itchy or painful. To flatten these scars and to limit the spread of keloids, treatment options at ETERNIS skin clinic are-
- Intralesional injection therapy
- Topical creams or gels – these help in combination with other treatment modalities
- Silicone gel sheets
- Pulsed Light therapy
- Surgery is not an ideal treatment for keloid as new keloid can appear over the surgery site.
What is Eczema?
Eczema (dermatitis) is an itchy rash with inflamed skin. Early, acute eczema can be red, blistering, or oozing and can appear anywhere. Later on, chronic eczema can be thickened, rough, and darker than the surrounding skin due to prolonged scratching.
Different types of eczemas depending on their cause are
Contact Allergic Dermatitis:
occurs due to contact with certain allergens e.g. metals, artificial jewellery, makeup, fragrances, rubber, hair dyes, adhesives in bindi, etc
Contact Irritant Dermatitis:
occurs due to contact with acids, alkalis, soaps, detergents. Commonly seen in house wives, maids, industrial workers
Photo-dermatitis:
eczema occurring on sun exposed parts of the body mostly seen in spring and summer.
Air Borne Contact Dermatitis:
Eczema occurring all over body due to allergy with congress grass (Parthenium). It is caused by airborne dry and friable particles of this plant. It usually appears in the spring and summers and often worsened by sunlight.
Atopic Eczema:
often starts in infancy and can extend in childhood or adult age. Such patients have history of frequent colds, asthma & dust allergy. It may run in families
Xerotic Eczema:
occurs due to dryness of skin especially in old age due to loss of moisture in the skin
Dyshidrotic Eczema (Pompholyx):
presents as extremely itchy tiny deep seated blisters on fingers, palms & soles. Tends to recur
What is Psoriasis?
Psoriasis is a common and chronic skin disorder that causes red, scaly and itchy patches on the limbs, trunk, scalp, nails and other parts of the body. Sometimes it causes joint pain and deformities. Psoriasis comes in many forms. Each differs in severity, duration, location, shape, and pattern of the scales. It is not a contagious disease.
What causes Psoriasis?
The cause is unknown. Triggers of psoriasis include a stressful event, sore throat, certain medications, cold weather, and trauma to the skin. Psoriasis is likely to occur in members of the same family.
How is it treated?
Psoriasis being a long standing disease needs a comprehensive management course over a long period of time to keep it under control (like diabetes). Every psoriasis patient is different and the treatment differs not only with the type of psoriasis, but also with the area involved, patient’s lifestyle, associated medical conditions and cost of the treatment. There are multiple treatments available like topical creams, oral medications, Phototherapy, Immuno-modulators and newer treatment like Biologics.
How do I take care of my skin if I have Psoriasis?
- Identify and control triggers (such as stress, certain medications, alcohol and smoking)
- Take care of your skin with plenty of moisturizer. Moisturizing creams and lotions loosen scales and help control itching.
- Avoid picking and scratching at the skin. New spots may appear 10 to 14 days after the skin is cut, scratched, rubbed, or severely sunburned.
- Do follow treatment regimen regularly as directed by dermatologist.
- Don’t give up treatments too soon as it may take a few weeks for some of them to work.
- Don’t indulge in self-pity and avoid people. Psoriasis is not contagious. Do not keep thinking about it. Mental stress only aggravates it
- Have a nutritious, balanced diet containing more green vegetables and sea food but less meat.
- Exercise regularly. Psoriasis is known to be associated with hypertension, diabetes and heart diseases. Best way to prevent these is by exercising and having nutritious balanced diet.
What is Vitiligo?
Vitiligo is an autoimmune condition in which white patches appear on the skin because of destruction of skin pigment cells called Melanocytes by the body’s immune cells. Vitiligo most commonly appears on areas exposed to the sun such as the hands, feet, arms, face, eyelids and lips. Vitiligo may spread slowly or rapidly to other parts of the body.
What causes it?
Till date the exact cause is still elusive. Vitiligo is worsened by severe sunburn, physical or emotional trauma. It is known to be associated with diseases of thyroid, anemia and diabetes.
How is it treated?
The society we live in has misconceptions about this disease and labels it as a stigma. Even in the present era of modern medicine, these patients find difficulty in getting married, face difficulty to get jobs and suffer social embarrassment. Vitiligo is just a condition causing change in the colour of skin with no harm to body and can be treated effectively if treatment started at early stage. Several treatment options are available for arresting the spread of vitiligo as well as restoring color in the white patches. Depending on the extent of involvement, treatment options include:
- Medical: Topical creams and oral medicines.
- Phototherapy: NB-UVB, PUVA (combination of medicine with ultraviolet light therapy)
- Surgical: Non-cultured melanocyte transfer, Skin grafting, punch grafting, blister grafting, tattooing of skin. View More
- Cosmetic: Camouflage creams to cover the white patches.
Tips for patients having Vitiligo:
- Vitiligo is not contagious and not evil. It doesn’t spread by touch.
- Practice sun protection using sunscreen and protective clothing.
- Reduce emotional and physical stress whenever possible by yoga, pranayam or by exercises you enjoy.
- Cultivate a habit you love and try not to think about your disease.
- While vitiligo may run in families, chance of getting vitiligo in children whose parents have the disorder is very less.
What is Urticaria/Hives?
Hives, or urticaria, are transient red lesions on the skin that often itch. These may appear anywhere on the skin and vary in size and shape. Most often, your hives will resolve within 24 hours or less. New hives may appear as older ones fade, so hives may last for a few days or longer. Hives generally lasts for less than 6 weeks (acute urticaria). When they persist beyond 6 weeks, it is called as chronic urticaria. Sometimes these lesions occur deeper in the skin, often causing swelling of eyelids or lips and difficulty in breathing (Angioedema).
What causes it?
Acute urticaria often results from an allergic reaction. Things that trigger an allergic reaction include recent infection, certain foods and food additives (citrus fruits, milk, eggs, cheese, chocolate, nuts, tomatoes and shellfish are common culprits), medications (mostly painkillers), dental caries, parasitic infestations, insect bites, new perfumes, hair dyes, detergents, lotions, creams, or new clothes, exposure to new pets, dust, chemicals, nickel, rubber or plants and rarely even Pregnancy. Other causes include exposure to sun, heat, cold or water, exercise, stress, pressure on the skin. Finding the cause of chronic hives can sometimes be very difficult.
How is it treated?
Treatment depends on the type of urticaria, its severity and how long it has been present. Sometimes laboratory blood tests may be needed to find out the probable cause especially in hives lasting for more than 6 weeks. The most common treatment is antihistamines. Antihistamines are anti-allergic medicines which relieve symptoms, such as itching. Occasionally, you may need a combination of multiple antihistamines to control the hives. Autologous serum therapy (AST) is a novel treatment option in chronic type of urticaria not responding to usual treatment. Other newer lines of treatment include Biologics and immuno-modulatory medicines.
What is Pruritus/Itch?
Pruritus, or itch, is an unpleasant sensation that provokes the desire to scratch. It can range in intensity from a mild annoyance to an intractable, disabling condition which can severely hamper the quality of life.
What causes Itch?
There are numerous causes of itch. It could be related to diseases pertaining to the skin or in certain cases diseases affecting various organs of the body. Generalized pruritus may be due to underlying causative diseases such as renal failure and in patients receiving hemodialysis (HD), liver diseases, hematologic conditions, chronic infections, endocrinological diseases, emotional stresses and some mental health disorders, certain medications, pregnancy related conditions and rarely even malignancies may be a cause.
How is it treated?
Primary skin disorders are excluded before a systemic cause is considered. A detailed history, physical examination and a systematic review of systems is needed with laboratory evaluation to find out the cause of the itch. In some cases a skin biopsy is needed for complete evaluation.
The treatment for pruritus varies depending on the underlying cause. It can include topical, oral medications & light based therapies like UV-B therapy.
Melasma
Melasma appears as a symmetrical blotchy, brownish black pigmentation on the face, often chronic and seen commonly in females. It’s seen in areas that receive excessive sun exposure. It occurs due to overproduction of melanin by the pigment cells of the skin. This condition often leads to considerable emotional distress.
What causes it?
The cause of melasma is complex. There is a genetic predisposition to melasma, with at least one-third of patients reporting other family members to be affected. Sun exposure is the most important avoidable risk factor. Pregnancy, Birth control pills, scented or deodorant soaps, toiletries and cosmetics or certain medicines may cause a phototoxic reaction triggering melasma that may then persist long-term. Also Ovarian and thyroid dysfunction are known to worsen it. Some patients also report lesion development or worsening after stressful events generating anxiety.
Is there any way I can Prevent it?
The adage ‘Prevention is better than cure’ is truly apt for the prevention of Melasma. Prophylactic management is often the most effective means of prevention. General measures include ‘year round’ strict sun protection with high SPF and PA rating sunscreen applied to the exposed areas daily, using a mild cleanser and light moisturizer. It is wise to include hats, umbrellas and protective clothings along with the sunscreen. Make-ups containing zinc oxide or titanium dioxide can also serve as protective and preventative therapy.
I have pigmentation on my face, is it Melasma?
Pigmentary disorders like Frictional melanosis, Acanthosis nigricans, Riehls melanosis, Ashy dermatosis or Lichen planus pigmentosus are common conditions which may mimic melasma. A thorough analysis by your dermatologist is preferable before starting any form of treatment.
How is it treated?
Management of melasma requires a comprehensive approach. Without the strict avoidance of sunlight, potentially successful treatments for melasma are doomed to fail. Melasma can be very slow to respond to treatment, sometimes taking months to see results. So don’t get disheartened if you don’t see immediate improvement. If you are on birth control pills, stopping these medications (after consultation with your doctor) may help fade the pigment. Skin lightening creams are the mainstay of treatment. We may also recommend certain chemical peels and laser treatments such as intense pulsed light (IPL) or Laser if your melasma is persistent.
Word of caution
Self medication with over the counter creams or medicines dispensed by medical stores and quacks often lead to worsening of melasma. These creams often contain potent steroids or bleaching agents which when used without supervision of a dermatologist lead to permanent damage to delicate facial skin.
What are stretch marks?
Stretch Marks, known medically as Striae are a type of atrophic scar presenting as lines or streaks on the skin. They can be pink, purple or white in colour and occur when the deeper skin layer is progressively stretched and loses its elasticity.
They are generally associated with puberty, pregnancy, obesity, bodybuilding and abuse of topical or oral steroid. It commonly occurs on the abdomen, hips, thighs, arms, back and breasts.
How are stretch marks treated?
Treatment is aimed at improving the skin texture of stretch marks and stimulating collagen formation in the deeper layers of skin.
Various treatment options available at ETERNIS skin clinic are:
- Microdermabrasion
- Electroporation
- Chemical Peels
- Fractional Laser Skin Resurfacing
- Micro needle radiofrequency
- Medical Skin Needling
- PRP Therapy
For Enhanced and Better results, combination of different procedures is preferred.
At Eternis clinic, we also provide Diagnostic and Therapeutic Management for –
Skin Conditions like:
- Viral infections like Warts, Molluscum, chickenpox, Herpes.
- Bacterial infections
- Fungal infections of skin, hair and nails.
- Scabies
- Leprosy
- Skin tuberculosis
- Rosacea
- Lichen planus
- Blistering disorders like Pemhigus, Pemphigoid, etc
- Autoimmune disorders like Dermatomyositis, Scleroderma, Lupus etc.
Diseases of oral mucosa and tongue
Nail disorders – Ingrown toe nail, nail infections etc
Diseases of male and female genitalia
Sexually transmitted diseases of males and females-
- Herpes genitalis
- Genital wart and Molluscum Contagiosum
- Bacterial STDs.

Pediatric Dermatology – Skin care of children
Compared to adults the skin of infants and children is more delicate and sensitive thereby needing special care and protection. There are certain skin conditions seen specially in kids like diaper dermatitis, ichthyosis, atopic dermatitis, bacterial and fungal infections, lice infestations, hemangioma, skin changes due to vitamin deficiencies as well as genetic and hereditary skin disorders. Dermatologists are well versed to diagnose and treat these conditions. Some of the commonly occurring disorders are:
Diaper Dermatitis (DD):
it is among the most common skin conditions seen in neonates and infants. It occurs when contact with urine and stool results in growth of bacteria and fungus and alters of the ph balance of the skin. All this contributes to compromised barrier function and dermatitis (skin inflammation). There is added risk of developing allergy to the cleansers used to cleanse the area. Using barrier creams, gentle cleansers is important to avoid DD. Sometimes anti-bacterial, anti-fungal and anti-inflammatory creams may be prescribed.
Pityriasis Alba:
it is a harmless, mild dermatitis seen as whitish patches, most often on cheeks. It can last for months with a tendency to recover spontaneously. Children having atopic dermatitis or dry sensitive skin are more prone. It is wrongly attributed to calcium deficiency, parasitic infestation or fungal infection in children. Some parents may wrongly worry that child has developed Vitiligo. In most cases treatment with moisturizers is sufficient. Excessive washing of the skin with soaps, self medication is to be avoided. If severe, anti-inflammatory creams may be prescribed.
Atopic Dermatitis:
often starts in infancy and can extend in childhood or adult age. It is characterized by dry and itchy skin. Such patients have history of frequent colds, asthma & dust allergy. It may run in families. These children are more prone to bacterial and viral infections in active phase of their eczema. They need special skin care to keep the disease under control which is very important for their physical and psychological wellbeing.
Cradle cap:
It is a type of seborrhoeic dermatitis in infants presenting as yellowish greasy scaling on crown area of scalp. It’s a form of fungal infection. Sometimes it may be associated with scaling on other body parts in which cases specific treatment may be needed. In mild cases application of baby oil before bathing is sufficient.
To know more on care of your baby’s skin, visit our experts at ETERNIS Skin clinic.
Women Skin Health
There are specific skin and hair disorders which exclusively affect women. At ETERNIS, our team of doctors, have expertise in correctly diagnosing these conditions and treat them effectively.
Hirsutism
It is a condition where excessive, thick hair growth is seen in women in areas such as face, neck, chest, abdomen and lower back. It is one of the most common endocrine disorders, affecting approximately 10% of women. Most times the cause is genetic and it’s more common in some ethnic race with no underlying disorder. However sometimes it may represent an underlying medical condition which may be serious also.
The primary reason for hirsutism is abnormal androgen hormone action, either in the form of excessive secretion of androgen hormones or increased sensitivity of hair cells to normal levels of circulating hormones in the body or both. Whatever the cause, this excess hair growth can result in emotional trauma and social embarrassment. Even mild cases of hirsutism may be viewed as a presumptive loss of femininity.
Treatment of hirsutism is aimed at finding out the cause and appropriate treatment for the underlying disorder. Cosmetic measures of hair removal in the form of mechanical depilation (shaving, plucking, waxing, depilatory creams) or light-based hair removal (laser or pulsed-light) are sufficient. In few cases long term oral medication is sometimes initiated along with cosmetic measures.
Poly cystic ovarian disorder
It is the most common disease affecting ovaries. It is characterized by formation of multiple cysts in the ovaries, menstrual irregularities, weight gain, and persistent elevation of sex hormones. Cutaneous manifestation are coarse hair growth ( hirsutism), persistent acne not responding to usual treatment, increased pigmentation over face and body folds and thinning of scalp hair with hair fall. It may also be associated with Metabolic Syndrome (diabetes, hypertension, abdominal obesity, high cholesterol levels). PCOS usually begins at puberty and is known to persist through adulthood. Treatment includes changes in lifestyle, dietary modification, medicines for metabolic syndrome and hormonal therapy.
Pregnancy related disorders
Pregnancy and motherhood are the most joyful moments in a woman’s life. But the footprints it leaves behind in form of stretch marks, lax skin, pigmentation- Melasma, hirsutism, post delivery hair fall may mar these joys. Timely management can help regain your confidence and self esteem. At Eternis clinic, we offer an array of treatments to take care of your skin while you take care of your little bundle of joy.
Skin disorders affecting female genitalia
The external female genitalia is called as Vulva. Many diseases affecting the vulva may present as a rash along with itching, burning sensation, pain or foul smelling vaginal discharge that can be caused by a number of health problems and should not be ignored. Without treatment, vulval conditions can lead to depression, anxiety, embarrassment, sexual problems and body image concerns. Some common conditions are due to infections, allergic contact dermatitis, pruritus vulvae, eczema, psoriasis, genital ulcers, lichen planus, Vitiligo, sexually transmitted diseases and rarely skin cancer. Treatment management may include culture swabs, smears, skin biopsy and blood tests.
Skin care tips to take care of your genital skin:
- Avoid soaps, detergents, antiseptics, powders, fragrant wipes, douches and bubble baths. Use ph balanced gentle non-soap cleanser and lukewarm water to wash the area.
- Avoid scented creams, perfumes and scented pads. You can use non-fragrant bland moisturizers if necessary.
- Keep area dry by gently patting dry the skin with soft toilet paper after passing urine.
- Avoid tight clothing, pantyhose and synthetic underwear. White cotton undergarments are preferred.
- Change pads/ tampons frequently (4-6 hourly) during periods.
- Avoid self medication. Seek medical help from a dermatologist in case you develop any skin rash or symptoms. Scratching the area and frequent cleaning will only worsen the condition.
- Perform regular self-examinations – it is helpful to use a hand mirror. Report any symptoms promptly to your doctor.
- Have plenty of water and probiotic foods like curd/buttermilk to maintain healthy lifestyle.